If you’re dealing with a chronic illness like mold toxicity, Lyme, or persistent inflammation, you’ve probably been told to “support your mitochondria” or “optimize methylation.” But what if part of your healing is stalling because a key nutrient—folate—isn’t making it to your brain?
That’s the case in a condition called Cerebral Folate Deficiency (CFD), where the brain ends up running low on 5-MTHF—a special, active form of folate—even when your blood tests show perfectly normal folate levels. This type of deficiency doesn’t happen from not eating enough greens. It happens because your body can’t transport the folate across the blood-brain barrier, where it’s needed for things like memory, mood, focus, and repair.
And one of the most overlooked reasons this happens is something we see all the time in complex chronic illness: mitochondrial dysfunction.
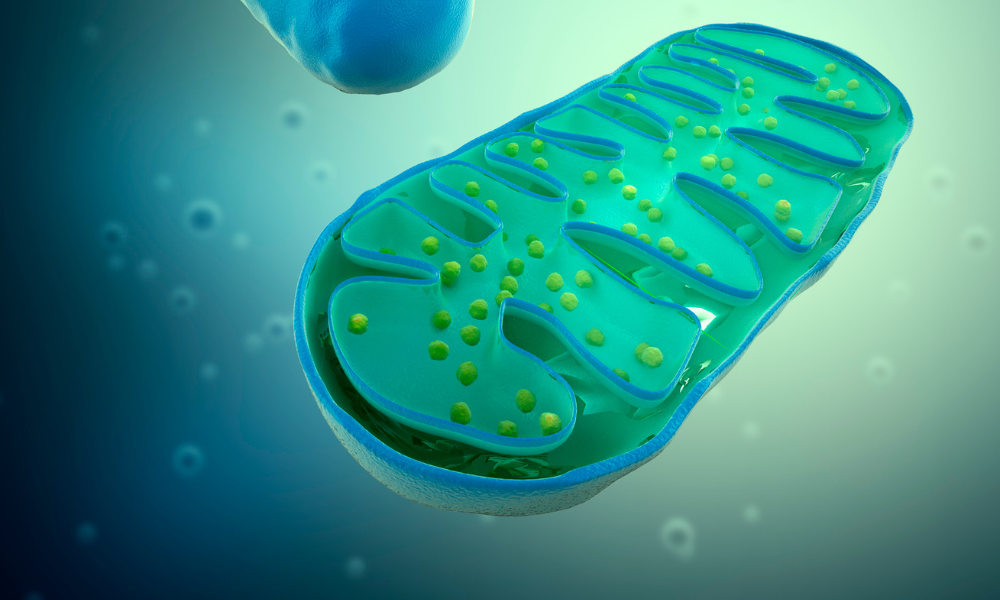
Wait—What Do Mitochondria Have to Do With Folate?
Mitochondria are tiny power plants inside your cells. They take nutrients and oxygen and turn them into ATP—the basic energy currency your body uses for everything from muscle movement to brain function. When mitochondria are running smoothly, your cells have the fuel they need to do their jobs. But when they’re stressed—by infections, toxins, inflammation, or just long-term illness—they start to underperform.
Here’s the catch: transporting folate into the brain isn’t a passive process. It actually requires energy—a lot of it. And that energy is supplied by—you guessed it—mitochondria. So if your mitochondria are running on fumes (as they often are in people with CIRS, mold illness, or vector-borne infections), your brain may not be getting the folate it needs, even if your multivitamin looks great on paper.
When Brain Folate Runs Low, So Does Function
Without enough folate in the brain, you can see a wide range of neurological symptoms:
- Brain fog or trouble focusing
- Anxiety, mood swings, or emotional sensitivity
- Trouble processing information or organizing thoughts
- Irritability or agitation (in both kids and adults)
- Poor sleep, sensory overload, or panic
In kids, this can look like regression, tantrums, or developmental plateaus. In adults, it often gets written off as anxiety or stress—but underneath, the brain may be under-fueled and under-supported.
And here’s the key: this isn’t necessarily because of genetics or poor diet. It’s often a downstream consequence of inflammation and energy collapse, especially in the context of chronic infections, toxic exposures, and persistent immune activation.
“Die-Off” or Mitochondrial Collapse?
If you’ve ever started a new antimicrobial or detox protocol and felt like your brain and body went into meltdown mode—days or even weeks of fatigue, fog, anxiety, or feeling emotionally unhinged—you may have been told, “It’s just a Herx reaction. That means it’s working.”
But that’s not always the full story.
What if these long, intense “die-offs” are actually evidence that your mitochondria couldn’t keep up with the metabolic demands of detox? What if your brain needed more folate to recover—but couldn’t get it because energy production had tanked?
This is where folinic acid and mitochondrial support can change the game.
Why Folinic Acid Matters
Folinic acid is a pre-converted form of folate—it doesn’t require the same enzyme steps or energy-intensive transport as other forms (like folic acid or even methylfolate). It’s like a pre-charged battery your brain can use right away, even if the mitochondria are struggling.
In patients with CIRS, mold toxicity, or chronic infections, I often recommend low to moderate doses of folinic acid (usually 800 mcg to 2 mg/day), especially if there are signs of neurological vulnerability. It supports:
- Brain repair
- Neurotransmitter balance (serotonin, dopamine, etc.)
- Methylation and detox pathways
- Emotional and cognitive regulation
And unlike synthetic folic acid, it doesn’t block folate receptors or build up unmetabolized in the blood. It’s well-tolerated in most, especially when paired with the right form of B12.
The Mitochondrial Basics: Support Without the Kitchen Sink
You don’t need to take 15 different supplements to support your mitochondria. For most patients, a focused approach using 3–4 key nutrients is enough to make a noticeable difference in energy, mental clarity, and recovery time after treatments.
Here’s what I start with:
1. Acetyl-L-Carnitine
Helps shuttle fats into mitochondria to be used for energy—especially helpful for the brain and nerves. Also supports mental clarity and repair.
Common dose: 500–1,500 mg/day
2. CoQ10 (Ubiquinol)
Acts as a spark plug in your mitochondria and protects them from oxidative stress. Low levels are common in chronic illness, especially if you’ve taken statins.
Common dose: 100–300 mg/day with food
3. Alpha-Lipoic Acid (ALA)
A powerful antioxidant that also helps regenerate other antioxidants like glutathione. Supports nerve health and glucose metabolism—especially useful in brain fog and fatigue.
Common dose: 300–600 mg/day
4. Magnesium (Glycinate or Malate)
Essential for making ATP and calming the nervous system. Low magnesium makes everything worse—fatigue, pain, sleep, stress tolerance.
Common dose: 200–400 mg/day
Start low, go slow, and adjust based on your tolerance and symptoms. Most people notice more stable energy, improved cognition, and fewer “crash and burn” detox days.
Can We Test for Mitochondrial Dysfunction?
Yes—but it’s not always necessary to start treatment.
Some mitochondrial-related nutrients (like CoQ10, carnitine, and RBC magnesium) can be measured through blood work. Organic acid testing (OAT) can show patterns of mitochondrial stress, like impaired energy production, fatty acid oxidation issues, or buildup of neurotoxic byproducts like methylglutaric acid.
There’s even more advanced testing like MitoSwab, which looks at how well each part of the mitochondrial energy chain is working—though that’s usually reserved for complex or refractory cases.
But in most people with CIRS, mold illness, or chronic infections, you don’t need to wait for perfect test results. The clinical picture—combined with symptoms—is often enough to start mitochondrial and folate support safely.
Final Thoughts
If you’ve been stuck in a cycle of “die-offs,” foggy brain days, or intense emotional reactivity every time you try to treat your root causes, it might not be that your protocol is too aggressive—it might be that your brain isn’t getting what it needs to recover.
Mitochondrial dysfunction can quietly block healing by cutting off energy at the cellular level. And when that happens, even the most basic nutrients—like folate—can’t reach the brain where they’re needed most.
Supporting your mitochondria and restoring cerebral folate isn’t about chasing symptoms. It’s about laying the groundwork for your brain and body to finally catch up and heal.
Sometimes, the missing piece isn’t a new diagnosis or supplement. It’s simply giving your cells the energy they need to do what they already know how to do.