When it comes to chronic illness—whether autoimmunity, ME/CFS, or biotoxin-related syndromes like CIRS or IACIRS—hormonal imbalances are common. But many patients and providers overlook a crucial mechanism at play: inflammation doesn’t just coexist with hormone dysfunction—it causes it.
One of the key culprits in this process is interleukin-6 (IL-6), a pro-inflammatory cytokine that plays a central role in immune signaling. IL-6 doesn't just reflect inflammation—it actively disrupts hormone regulation across multiple systems. At the same time, hormones can also influence IL-6 levels, creating a feedback loop that’s especially relevant in long-term illness.
Understanding this bidirectional relationship provides a missing link for patients whose symptoms don’t line up neatly with their lab results—and offers a more effective roadmap for recovery.
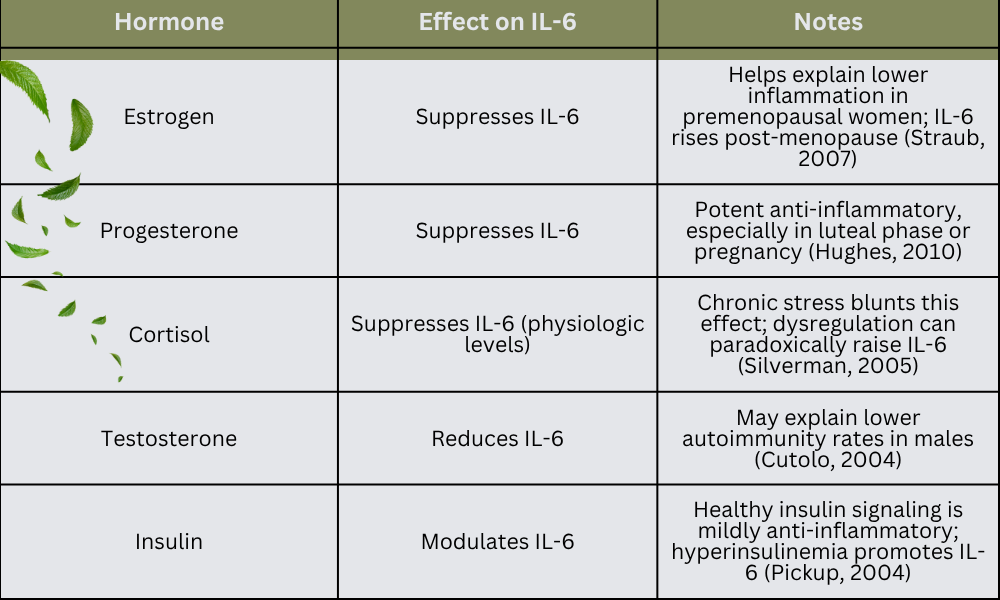
🔁 How Hormones Affect IL-6
Several key hormones help regulate inflammation by modulating IL-6 production. When these hormones are in balance, they can help keep inflammation in check. When they are deficient or dysregulated, IL-6 often rises.
🔄 How IL-6 Affects Hormones: A Deeper Look
Once IL-6 levels are chronically elevated—whether due to unresolved infection, toxin exposure, or immune dysregulation—it begins to interfere with hormone signaling across the body. This can lead to multi-system symptoms and patterns that don’t always show up clearly on labs.
IL-6 stimulates the hypothalamic-pituitary-adrenal (HPA) axis, initially increasing cortisol production. But over time, this constant demand can flatten the cortisol curve or contribute to adrenal dysregulation, leading to fatigue, poor stress resilience, and disrupted sleep-wake cycles.
It also suppresses the hypothalamic-pituitary-gonadal (HPG) axis, reducing signals that regulate sex hormone production—resulting in lower levels of estrogen, progesterone, and testosterone. This explains why so many patients with chronic inflammation experience mood changes, libido loss, irregular cycles, or early perimenopausal shifts.
In addition, IL-6 increases aromatase activity, promoting conversion of testosterone to estrogen. This can lead to a state of relative estrogen dominance—not necessarily from excess estrogen, but from disproportionately low progesterone and testosterone. This hormonal skew contributes to anxiety, poor sleep, and heightened histamine sensitivity.
IL-6 also increases sex hormone–binding globulin (SHBG), which binds to and inactivates circulating hormones. Even with “normal” total hormone levels, patients may feel symptomatic due to reduced free hormone availability.
Finally, IL-6 impairs thyroid hormone regulation by reducing TSH output and interfering with T4-to-T3 conversion. The result is often a low free T3 with normal TSH—a classic pattern in chronic illness, even when the thyroid gland itself is structurally intact.
🧪 Supplements That Support Hormone Recovery by Reducing IL-6
While treating root causes—such as environmental toxins, infections, and stress—is essential, some evidence-based supplements can help reduce IL-6 and support more efficient hormone recovery. These tools may help speed up symptom resolution when integrated into a broader functional medicine strategy.
🌿 1. Curcumin (Turmeric Extract)
- Mechanism: Inhibits NF-κB and IL-6 signaling.
- Dosing: 500–1000 mg/day with black pepper extract or liposomal formulation.
- Panahi et al., 2016
🫐 2. Quercetin
- Mechanism: Flavonoid, mast cell stabilizer, broad anti-inflammatory.
- Dosing: 500–1000 mg/day.
- Li et al., 2016
🧈 3. Omega-3 Fatty Acids (EPA/DHA)
- Mechanism: Lower IL-6 and CRP via eicosanoid signaling.
- Dosing: 1000–3000 mg/day (triglyceride or re-esterified form).
- Calder, 2013
🥬 4. Resveratrol
- Mechanism: Activates SIRT1 and reduces IL-6.
- Dosing: 200–500 mg/day.
- Poulsen et al., 2013
🍄 5. Reishi (Ganoderma lucidum)
- Mechanism: Reduces IL-6, TNF-α, and IL-1β.
- Dosing: 1000–2000 mg/day (standardized extract).
- Wachtel-Galor et al., 2011
🧘♀️ 6. L-Theanine
- Mechanism: GABAergic calming, reduces stress-induced IL-6.
- Dosing: 100–400 mg/day.
- Unno et al., 2013
🔋 7. Alpha-Lipoic Acid (ALA)
- Mechanism: Antioxidant, mitochondrial support, lowers IL-6.
- Dosing: 300–600 mg/day.
- Ziegler et al., 2004
☀️ 8. Vitamin D
- Mechanism: Suppresses IL-6 gene expression.
- Target: 25(OH)D levels between 50–70 ng/mL.
- Yin & Agrawal, 2014
🧠 9. Probiotics (Select Strains)
- Mechanism: Modulate gut-immune signaling to reduce IL-6.
- Key strains: Lactobacillus rhamnosus GG, Bifidobacterium longum.
- Cristofori et al., 2021
🔍 Final Thoughts
Hormone imbalances in chronic illness are often downstream effects—not root causes. And in many cases, IL-6 is the missing link between immune activation and endocrine disruption. Instead of chasing isolated hormone panels, it’s often more effective to reduce the inflammatory drivers that are disrupting hormonal control in the first place.
This is where integrative strategies that address infections, toxins, nervous system stress, and mitochondrial resilience truly shine. Hormonal recovery doesn’t always require direct replacement therapy—it often starts by restoring immune balance and allowing the body’s own regulatory systems to recalibrate.
Targeted supplements can help speed the process, but the foundation remains the same: lower inflammation, support detox, stabilize the system—and let the hormones follow.
🧾 References
- Calder, P. C. (2013). Omega-3 polyunsaturated fatty acids and inflammatory processes: nutrition or pharmacology? British Journal of Clinical Pharmacology, 75(3), 645–662. https://doi.org/10.1111/j.1365-2125.2012.04374.x
- Cristofori, F., Dargenio, V. N., Dargenio, C., Miniello, V. L., & Barone, M. (2021). Anti-inflammatory and immunomodulatory effects of probiotics in gut inflammation: A door to the future. Frontiers in Immunology, 12, 622934. https://doi.org/10.3389/fimmu.2021.622934
- Cutolo, M., Capellino, S., Sulli, A., Serioli, B., Straub, R. H. (2004). Estrogens and autoimmune diseases. Annals of the New York Academy of Sciences, 1051, 525–536. https://doi.org/10.1196/annals.1361.048
- Hughes, G. C. (2010). Progesterone and autoimmune disease. Autoimmunity Reviews, 9(8), A247–A252. https://doi.org/10.1016/j.autrev.2009.12.007
- Li, Y., Yao, J., Han, C., Yang, J., Chaudhry, M. T., Wang, S., Liu, H., & Yin, Y. (2016). Quercetin, inflammation and immunity. Nutrients, 8(3), 167. https://doi.org/10.3390/nu8030167
- Panahi, Y., Khalili, N., Sahebi, E., Namazi, S., Reiner, Ž., & Majeed, M. (2016). Curcuminoids modify lipid profile in type 2 diabetes mellitus: A randomized controlled trial. Complementary Therapies in Medicine, 27, 1–5. https://doi.org/10.1016/j.ctim.2016.03.004
- Pickup, J. C. (2004). Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Diabetes Care, 27(3), 813–823. https://doi.org/10.2337/diacare.27.3.813
- Poulsen, M. M., Vestergaard, P. F., Clasen, B. F., Radko, Y., Christensen, L. P., Stødkilde-Jørgensen, H., Møller, N., Jessen, N., Pedersen, S. B., Jørgensen, J. O. L. (2013). High-dose resveratrol supplementation in obese men: an investigator-initiated, randomized, placebo-controlled clinical trial of substrate metabolism, insulin sensitivity, and body composition. Diabetes, 62(4), 1186–1195. https://doi.org/10.2337/db12-0975
- Silverman, M. N., Pearce, B. D., Biron, C. A., & Miller, A. H. (2005). Immune modulation of the hypothalamic-pituitary-adrenal (HPA) axis during viral infection. Viral Immunology, 18(1), 41–78. https://doi.org/10.1089/vim.2005.18.41
- Straub, R. H. (2007). The complex role of estrogens in inflammation. Endocrine Reviews, 28(5), 521–574. https://doi.org/10.1210/er.2007-0001
- Unno, K., Noda, S., Kawasaki, Y., Yamada, H., Morita, A., Iguchi, K., ... & Hoshino, M. (2013). Reduced stress and improved sleep quality caused by green tea are associated with a reduced caffeine content. Nutrients, 5(10), 4412–4422. https://doi.org/10.3390/nu5104412
- Wachtel-Galor, S., Yuen, J., Buswell, J. A., & Benzie, I. F. F. (2011). Ganoderma lucidum (Lingzhi). In Herbal Medicine: Biomolecular and Clinical Aspects (2nd ed.). CRC Press/Taylor & Francis. https://www.ncbi.nlm.nih.gov/books/NBK92757/
- Yin, K., & Agrawal, D. K. (2014). Vitamin D and inflammatory diseases. Journal of Inflammation Research, 7, 69–87. https://doi.org/10.2147/JIR.S63898
- Ziegler, D., Ametov, A., Barinov, A., Dyck, P. J., Gurieva, I., Low, P. A., ... & Samigullin, R. (2004). Oral treatment with alpha-lipoic acid improves symptomatic diabetic polyneuropathy: the SYDNEY 2 trial. Diabetes Care, 29(11), 2365–2370. https://doi.org/10.2337/diacare.29.11.2365